My Blood Clot Diagnosis and Treatment from the U.S. Healthcare System
- Mickey Ferri
- Oct 25, 2018
- 9 min read
Updated: Apr 30, 2019
I recently suffered a blood clot at age 33. I was diagnosed and treated by the U.S. healthcare system, which was a frustrating and time-consuming experience.
In this post, I give a brief account of my injury and symptoms, and I discuss in detail my diagnosis and treatment from the U.S. healthcare system. For a full account of how I sustained the blood clot, check out: "My September 2018 Blood Clot Injury."
This post has 7 short sections: (1) My injury and symptoms, (2) My initial visit to the MD, (3) The Healthcare "Game of Telephone," (4) My Ultrasound appointment, (5) Anticoagulants, aka "Blood thinners," (6) The big picture, and (7) How you can help.
I've been fortunate to be relatively healthy in my life, and I imagine others may have even more severe stories. Do you have a "United States healthcare story" to share? If so, you can share by filling out the form at Economics Athletes: My Healthcare Story, or reach out to us at hello@econathletes.com.
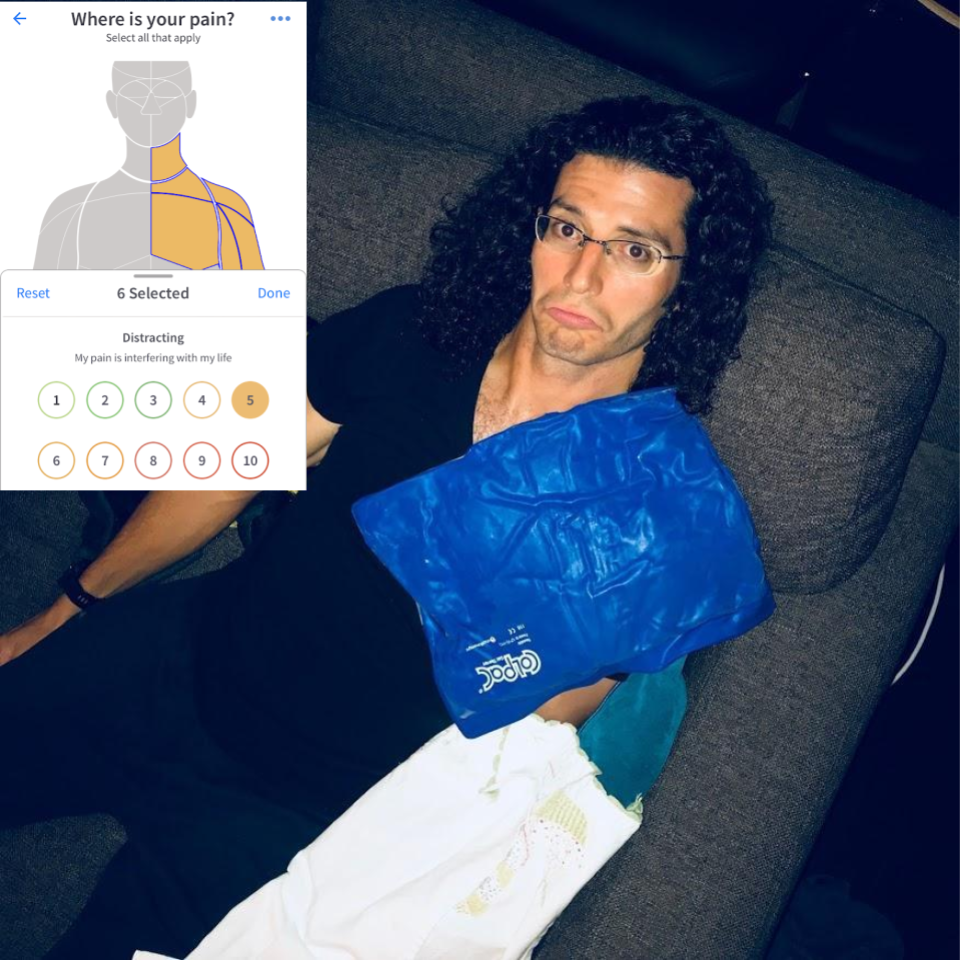
1. My Injury and Symptoms
After sustaining a serious injury on or around September 9th during a 5k race, I experienced intense pain down the entire left side of my body, head to toe.

After the race, there was some pain and swelling in my left arm. It seemed to me like a bad muscle strain. I didn't know anything about blood clots, so I treated it like a muscle strain, iced it, and it started to feel better.
I tried to book an appointment with my MD, and the earliest I could get on his schedule was over 2 weeks away! At the time, I didn't realize the severity of my injury, so I just waited. I figured: my MD is pretty busy, I'm pretty busy, we have a shortage of doctors in the U.S., so I won't take up his valuable time.
One odd symptom remained, however: blood didn't seem to be getting all the way through to my left arm...
2. My Initial Visit to the MD
October 3, 2018. I saw my primary care MD (over two weeks after I scheduled the appointment). He suspected a possible blood clot, so we scheduled an Ultrasound and X-Ray as soon as possible.
October 10, 2018. My ultrasound appointment was scheduled for one week away, which was "as soon as possible."
3. The Healthcare "Game of Telephone"
What ensured starting October 3 seemed like a convoluted and nightmarish version of the children's game called "Game of Telephone" aka "Chinese Whispers." Do you remember that game? It's where players form a line, the first person comes up with a message and whispers it into the second player's ear, and so on down the line, until it gets to the end. Then the last player shouts the message out loud. The message usually is different from the original, which is funny in the game. However, in real life when a person's health and life are at stake, it is not amusing.
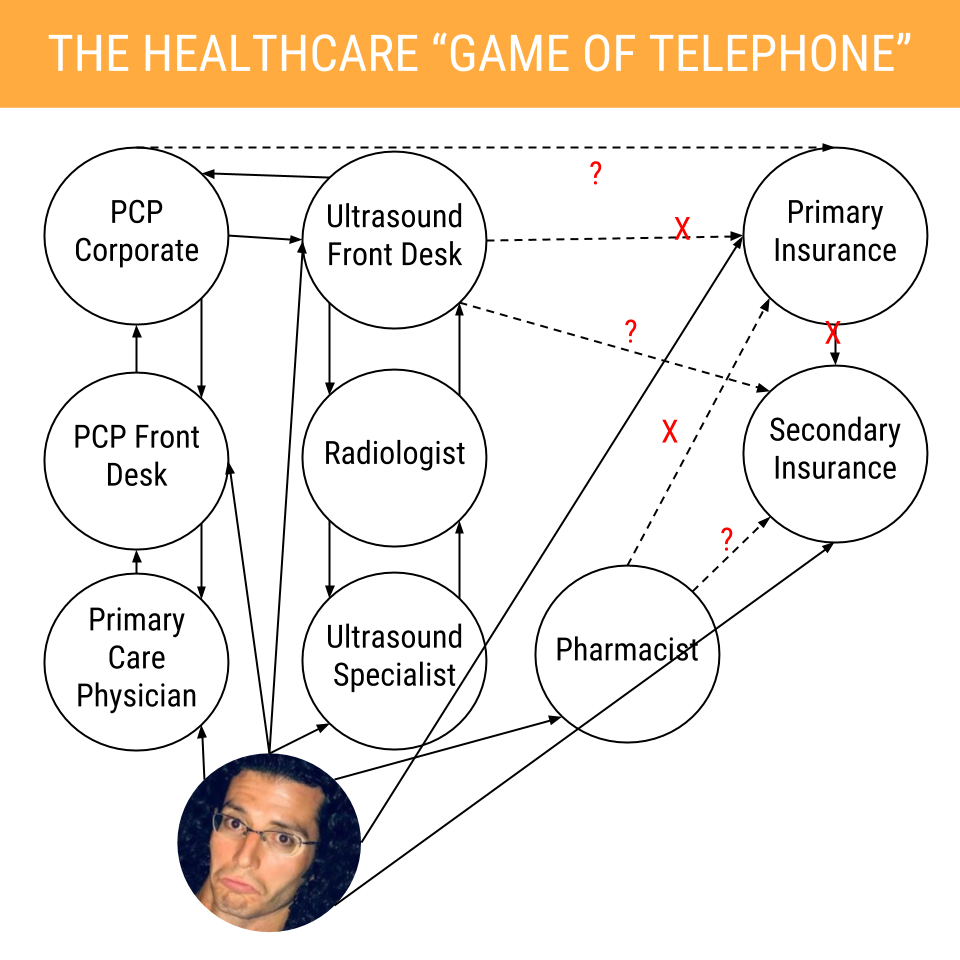
While reading the below description, keep in mind that my primary care physician, ultrasound specialist, and pharmacist are all located within 0.5 miles of each other, virtually on the same street in San Diego, CA.
4. My Ultrasound Appointment
Here's how scheduling, completing, and paying for the ultrasound went:
October 3, 2018. My primary care physician (PCP) told his front desk I need an Ultrasound.
PCP front desk notified PCP corporate electronically I need an Ultrasound.
PCP corporate notified an Ultrasound specialist down the street I need an Ultrasound.
I called the Ultrasound specialist to schedule an appointment ASAP. I was in their system, so I could schedule. The earliest available was one week away. I told them it was a serious and potentially life threatening condition, and they said one week was the earliest unless I went to the ER and waited, potentially for many hours. I booked the appointment for October 10.
PCP corporate notified my primary insurance company I have a serious medical condition which required an ultrasound.
My primary insurance company does not cover Ultrasound, they attempted to notify my secondary insurance company (which may cover Ultrasound) that I need one
The secondary insurance company didn't answer the phone, is only open 9am-3pm PT, and only accepts fax machine requests.
No one followed up on this notification, while I was under the impression someone was working to get my treatment covered by insurance.
October 10, 2018. I visited the ultrasound location and checked in at the front desk.
I was told that despite attempts to reach the insurance companies, it was unclear which of my two insurance companies, if any, were supposed to cover my treatment, and it was not going to be covered. I paid $200 cash for the Ultrasound treatment, and I am still attempting to get reimbursed as of October 24.
Meanwhile, I was assured that my scheduled X-rays were "definitely going to be covered." X-rays there are simple and quick and don't require an appointment in advance at this location.
I saw an ultrasound specialist for a 40 minute exam. During the exam, I asked her a few questions. She was very kind and clearly wanted to help. However, she informed me that she was strictly not allowed to give me any specifics on the test results - only the Radiologist (her boss) could, after the exam. She finished the exam and I left the room.
I saw a separate X-Ray specialist, who took chest X-Rays. This only took a few minutes.
When I came out of the X-Ray room, the woman from the front desk, frantic, told me that she had not been able to get ahold of my insurance company, and that it turns out the X-ray was not covered. She apologized profusely, which I appreciated.
I waited around for the radiologist to give me the ultrasound and X-ray test results.
The Ultrasound specialist came out and told me that while the radiologist had reviewed my results, he was unavailable to speak to me. He would (1) send the information to the front desk, who would (2) send it to my primary care corporate office, who would (3) send it to my primary care front desk, who would (4) send it to my primary care doctor.
I left the office and went home, not knowing anything of the results or my condition.
In the meantime, I attempted to get this procedure covered. I called my primary insurance company. After 30 minutes on hold, they told me that it was actually the secondary insurance company I had to call...their phone number is not on my card or anywhere I could find it. The primary insurance company gave me the secondary insurance company's number.
I called the secondary insurance company. No answer, and it went to a strange noise.
I hung up and called again. After several minutes, the secondary insurance company answered. They had my name and basic information on file, yet they had zero information about the recent doctor visit and request for ultrasound. They told me I would need to call my PCP front desk and have them fax the request to a fax number which is not listed on their website or anywhere else I have seen. I got the fax number from this secondary insurance company.
I called my PCP front desk, who took down the fax number. They told me that while they do not fax it directly to the insurance company, they would inform my PCP corporate, who would put in the request.
5. Anticoagulants, aka "Blood thinners"
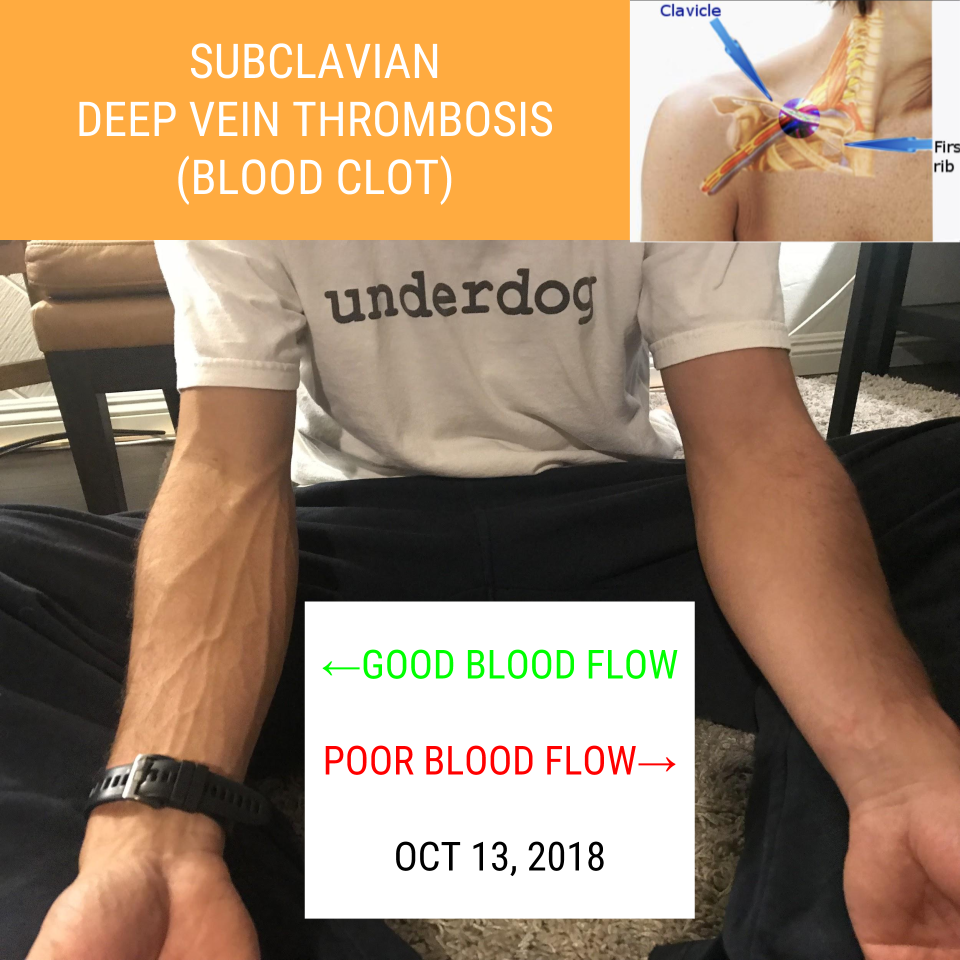
October 12, 2018. My doctor saw the ultrasound test results (48 hours after the test had been administered) and urgently called me, insisting I come in to the office immediately. I came in, he informed me I had a subclavian blood clot, (aka Subclavian Deep Vein Thrombosis, DVT) on my left side, under my collarbone.
The clot is in a dangerous spot in my body. The risk is the clot could dislodge, travel to my lungs, heart, or brain, and cause serious problems meaning a heart attack, a stroke, a visit to the ER, or death. The good news is it’s a relatively small blood clot so if I take it easy it should clear up and I should be ok after a few weeks.
The doctor recommended I take anticoagulants aka "blood thinners," starting immediately and continuing until the clot dissipated. Specifically: 15 mg pills twice a day for 3 weeks, then 20 mg pills once a day for another four weeks. Then we would do another ultrasound to see if the clot was gone. Sounded reasonable to me.
"Blood thinners" don't actually thin your blood, they prevent new clots from forming. Yes, that is confusing and it confused me as well, so I prefer to call them anticoagulants.
The anticoagulants normally cost about $20 per pill, which would have cost me ~$840 for the first three weeks and an additional $504.99 for the next four weeks, a total of ~$1,344.99 for the full seven weeks. Maybe the insurance companies would cover this...? Fortunately I didn't have to find out. Thanks to free samples and pharmaceutical coupons, I paid zero dollars for all these pills!
My doctor gave me the first 3 weeks worth of free samples, which they just happened to have laying around the office.
I started taking the anticoagulants, and I felt no negative side effects, aside from some mild dizziness one night.
October 23, 2018. I went for my check-in appointment with the doctor. Things are looking good. I was advised that the clot seems to be breaking up, and I can resume to semi-normal activity, just don't push it too hard, get stabbed, or bump into anything that could cause major bleeding or a major bruise. If so, I could develop internal bleeding, and the anticoagulants prevent the bleeding from stopping, which could mean a trip to the ER.
The MD put in a prescription to the pharmacist (down the street) for 30 more pills to take me through another month, and he gave me a paper card with a discount code that he advised "may" help with the insurance coverage.
I visited the pharmacist to fill the prescription. The pharmacist informed me that the bottle of pills would cost $504.99 for 30 days. He put in a request to the insurance company for coverage, yet it was DENIED. He put in the discount code, which was also DENIED.
The pharmacist said he would have to call the insurance company for "prior authorization," and we may have to call my doctor as well, so I waited around while he waited on hold with the insurance company...he never actually got through...
In the meantime, about five minutes later, the pharmacist was looking around the pharmacy, and he found a special coupon from the pharmaceutical company that enabled him to give me the $504.99 bottle of 30 pills FOR FREE. He said "oh wow, we got lucky, it's the last one, I didn't think we had any of these..."
He scanned the coupon, hung up the phone, and I checked out of CVS paying $0.
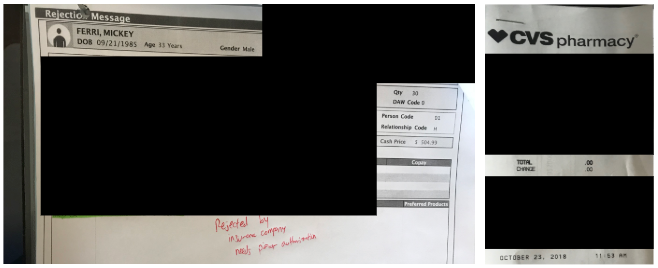
While I appreciate that I did not have to pay any money for the $1,344.99 worth of pills, I find it very concerning that this was only due to a two lucky things falling into place for me at the right time: (1) my doctor having enough free samples and (2) my pharmacist having a coupon laying around. The experience could have been very different.
6. The Big Picture
When I got home from the pharmacist, there was a package sitting on my front doorstep, delivered from Amazon.com, my favorite store. I ordered the package about 24 hours before it arrived, with one simple search and one click on my smartphone in about 30 seconds. By some miracle Amazon had it there the next day.
That miracle is similar to "the invisible hand" in economics. The invisible hand works well when systems are (1) vertically integrated, (2) trusting, and (3) everyone's incentives are aligned. Amazon.com demonstrates that multi-billion dollar operations can be run efficiently.
In contrast to Amazon, my experience with U.S. healthcare was quite the opposite. It was frustrating and inefficient.
I wonder:
Am I alone, or has anyone else had a negative experience with U.S. healthcare?
How much room for improvement is there in U.S. healthcare?
How can we fix it?
Unfortunately, based on the research I've seen, the best answers out there now are:
You're not alone.
"Umm...what?"
"No one really knows..."
Research from the RAND Corporation indicates that "Efficiency measures have been subjected to few rigorous evaluations of reliability and validity, and methods of accounting for quality of care in efficiency measurement are not well developed at this time." (emphasis in bold added).
Research from the medical community indicates that "Further research is needed for measurement of health care efficiency to advance and become accepted."
In one example, the Bloomberg Health-care efficiency index ranked the U.S. 54th out of 56 countries that were assessed (almost worst in the world).
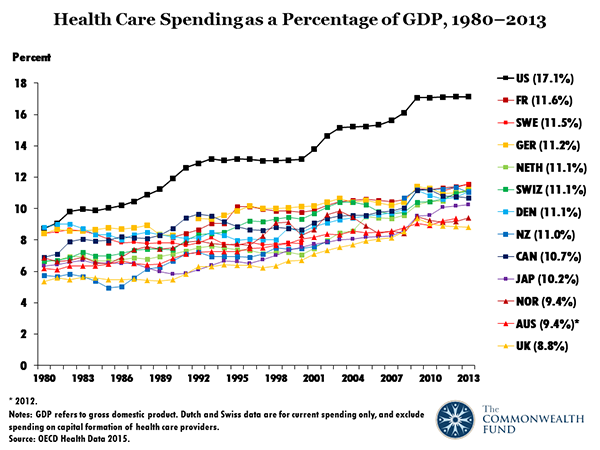
One thing we do know is that we spend a lot of money on healthcare. Data from the Center for Medicare and Medicaid Services indicate that U.S. healthcare costs are much higher than in other countries. I've included some of the key charts and statistics below, and you can see this presentation for more. U.S. Healthcare spending in 2016 was $3.3 trillion, or $10,348 per person, and represented 17.9% of our GDP. As a share of GDP, that's about double what it was in 1980.
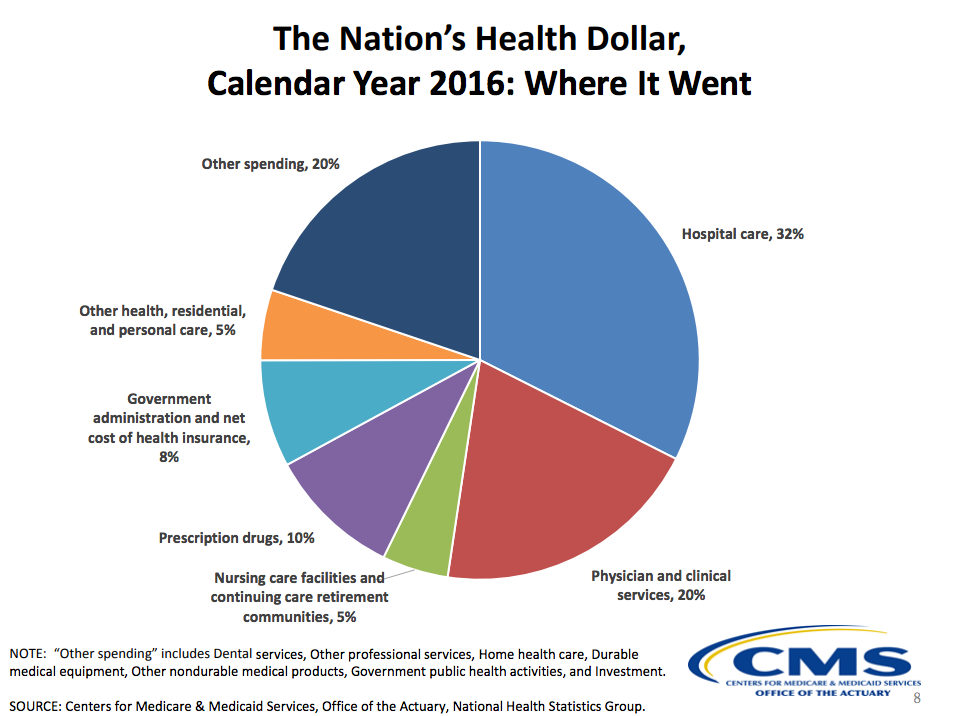
Here's an overview of where the money went in 2016. This touches on which areas we can look to for potential gains in efficiency.
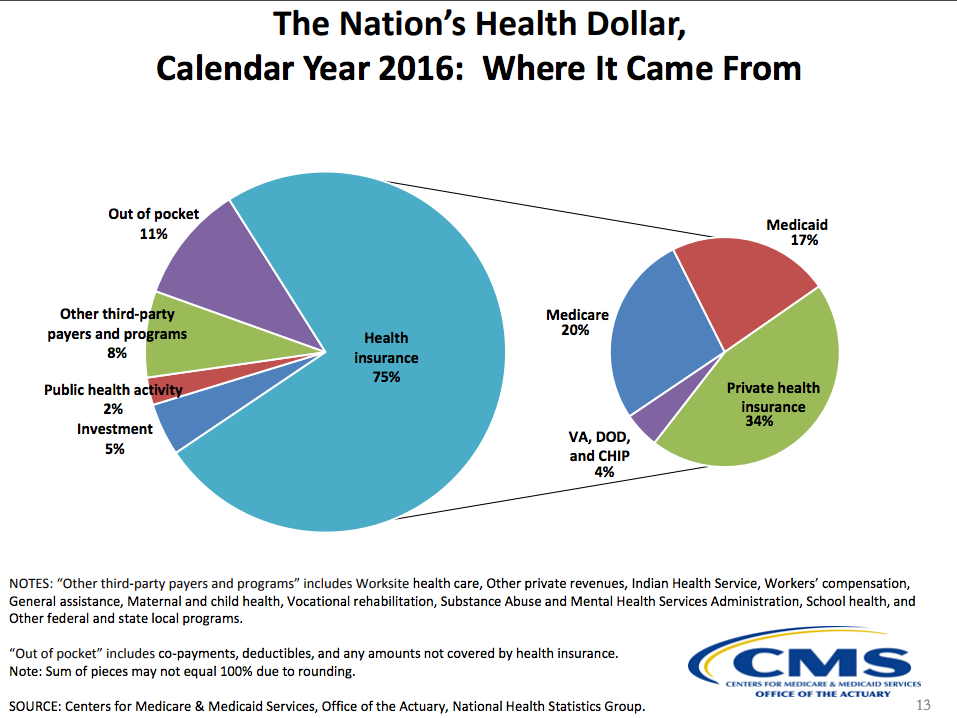
Here's an overview of who paid for it in 2016. This touches on who the big players are where we need to understand incentives well.
Estimates of healthcare expenditures that are wasted and/or unnecessary in the United States range from 20% to 33% or 34%. Examples of "waste" include: 1. Failure to deliver services, 2. Failure to coordinate care, 3. Over-treatment, 4. Administrative costs, 5. Pricing failures, 6. Errors, and 7. Pricing failures.
7. How You Can Help
Want to help improve our healthcare system?
First, this is a big issue with many stakeholders who may have diverse needs and opinions that need to be valued. Second, whatever we do, we should not to expect to see improvements overnight. I encourage you to be persistent, yet also patient. Third, by sharing information and opinions in a constructive way, I think we will start to see more data and improvements over the long-term.
Here are three things you can do now that may make a positive difference.
Visit https://allofus.nih.gov/ and join the "All of Us" research program.
If you have a story to share, please fill out the Economics Athletes: My Healthcare Story survey.
Share this blog post with others and help spread the word. Without awareness, we have no hope of real change.
Until next time,
~Mickey






Comentários